Intro to Polyvagal Theory
The two branches of the Parasympathetic Nervous System
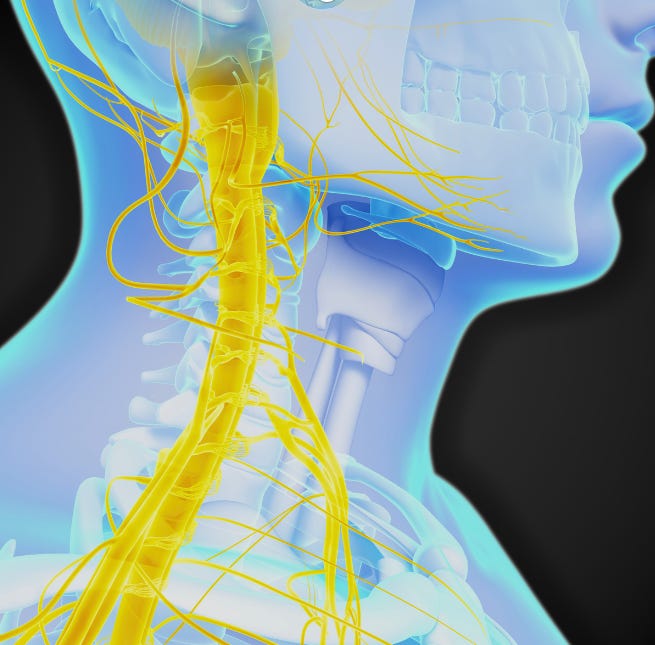
The vagus nerve is the chief conductor of parasympathetic signals from the brain to the body, and as such it plays a major role in restoring physiological homeostasis after experiencing an acute stress response. While the term “parasympathetic signals” makes it sound like the vagus nerve communicates a single message to the body (slow down and relax), there are actually four different nuclei, or bundles of cells in the brainstem, into which the vagus nerve plugs in. Two of these mainly carry efferent (brain-to-body) pathways, and so the brain may trigger each of these pathways separately or simultaneously or neither.
The name of these two nuclei are as follows:
the dorsomotor nucleus
the nucleus ambiguus
The dorsomotor nucleus contains visceral efferent nerves that signal to the abdominal viscera to carry out activities to benefit the organism. These activities include secretions of enzymes, hormones, fluids, and smooth-muscle contractions like those that move food through the intestines. The dorsomotor nucleus also contains motor efferents to the heart and lungs. Signals to the heart from the dorsomotor nucleus slow it down, and signals to the lungs cause the bronchioles (small airways) to constrict in order to preserve moisture and reduce turbulence, making gas exchange in the lungs steadier. Because of the critical role the the signals from the dorsomotor nucleus play in facilitating digestion in the organism, the portion of the vagus nerve originating from the dorsomotor nucleus has sometimes been given the name the “vegetative” vagus. Another word used is the dorsal vagus complex (DVC), so-named after the dorsomotor nucleus.
The nucleus ambiguus has motor neurons to the various thoracic organs, including the heart, lungs, pharynx, larynx, mouth, nasal region, and other parts of the head including the middle ear and tear ducts. Its activity increases when we perceive the environment as safe, and therefore a place where we can open up to and interact with others in a supportive way. This nucleus and system of neurons, sometimes called the ventral vagus complex (VVC), has two important functions. Its main functions are to act as the chief parasympathetic brake on the heart rate, and to promote social engagement through potentiating nerve pathways related to interacting with others (more on both of these later).
Even though both nuclei can lower the heart rate, the nucleus ambiguus plays the chief role of regulating heart rate in mammals during day-to-day activity. And unlike the nerves of the dorsomotor nucleus, the nerves within the portion of the vagus nerve originating from the nucleus ambiguus have what is called myelination. Myelination is a coating that provides electrical insulation to the nerves and increases their signal speed up to three hundred times faster. Because of the position of the nucleus ambiguus is ventral (“in front”) relative to the dorsomotor nucleus in the medulla, this system of myelinated nerves originating from it is called the “ventral vagus complex” (VVC).
Function of the Ventral Vagus Complex (VCC)
With its rapid signal transmission due to myelination, the ventral vagus complex acts as the main parasympathetic brake to the heart, counteracting the activity of the sympathetic nervous system. Another term given to the VVC is the “smart vagus,” due to its role in dynamically controlling the heart rate in response to breathing. Each inhalation takes air into the lungs and inflates the several hundred million microscopic air sacs, called aveoli, which are lined with blood capillaries and where the blood absorbs oxygen and off-gases carbon dioxide and other metabolic waste products. The VVC modifies the heart rate so that optimal blood flow for gas exchange within the lungs occurs at the precise moment the aveoli are at maximum ventilation.
This ongoing beat-to-beat modulation of the heart rate, synchronized with the rhythm of respiration, is called respiratory sinus arrhythmia, or RSA for short. In clinical settings, having a pronounced respiratory sinus arrhythmia is a sign that the ventral vagus nerve is functioning healthfully and coordinating the respiratory and cardiovascular systems of the body for optimal gas exchange and tissue oxygenation.
Although the VVC’s direct stimulation of the heart lowers heart rate, the VVC’s activity rapidly increases and decreases, allowing it to indirectly raise the heart rate through the removal of its activity as a “vagal brake” without any need to directly activate the sympathetic nervous system itself.
We as mammals, being warm-blooded and producing our own body heat, require a lot of energy and oxygen for our day-to-day functioning. Because of this, the consistent stimulus of the ventral vagus complex, facilitated by a sense of safety in the environment, helps promote and maintain consistent energy levels in our body, even at levels of activity comparatively lower than those typical of the fight-or-flight response. It does this through this respiratory sinus arrhythmia.
The second function of the “smart vagus” is to promote social engagement with others by encouraging the muscles in our head, face, and voicebox to activate. All these muscle groups have to do with social interaction. When we feel safe and relaxed we make more eye contact with people, turn our heads to them, make more facial expressions, and even our voice has more intonation and song-like quality (prosidy). Having lots of time with friends and family is one of the best predictors of longevity, because these interactions increase our sense of safety, and actually promote greater relaxation, digestion, and even memory and creativity.
Function of the Dorsal Vagus Complex (DVC)
Contrasting this, the dorsal vagus complex (DVC) can slow the heart down, but it does so in a much clumsier and dramatic fashion, suppressing sympathetic activation to a much stronger degree. The expression of dorsal vagal signally is more pronounced in a number of states, of which can present independently of the activation of the ventral vagus complex, its gentler heart rate brake, and its priming of the body to engage socially with others. Some of these states include:
deep states of rest, sleep, or “food comas”
seasonal states of torpor, lethargy, or hibernation
spells of fainting, induced by shock and by a sudden drop of blood pressure to the brain
states of suppression or cessation of breathing (e.g. the mammalian dive reflex)
states of immobilization, passive avoidance, or death-feigning
A variety of these states present as a result of the DVC lowering the heart rate and lung ventilation, resulting in a reduced metabolism. The DVC releases oxytocin, which mitigates the effects of the adrenaline and cortisol, similar to the VVC, which further dampens the propensity for activity. Large amounts of signaling via the DVC are used for the secretion of digestive enzymes and to move food through the alimentary canal of the body, particularly after larger meals.
What neonatal care teaches us about the nervous system
The above analysis of the dual motor branches of the vagus nerve, termed the Polyvagal Theory, was first put forth by Dr Stephen Porges, who is a professor of psychiatry and the director of the Brain-Body Center at the University of Illinois at Chicago.
Among many things, he was known for the pioneering a means of quantifying the measurement of heart rate variability (HRV), or beat-to-beat changes in the heart rate.
Prior to the discovery of a robust way to measure HRV, heart rate itself was used primarily as a marker for determining one’s physiological state. Because this is a uni-dimensional variable attempting to describe the activity of two separate influences, the sympathetic nervous system and parasympathetic nervous system, the ability to tease out which effects were the result of which influence was a challenging process. Our ability to understand concepts like arousal, stress, and autonomic balance between the two systems could only be incomplete. With the discovery of heart rate variability as mediated by the vagus nerve, sometimes equivocated with “vagal tone,” the individual contributions of the sympathetic and parasympathetic nervous systems to heart rate could be independently ascertained.
From this a paradox emerged.
As mentioned before, heart rate variability is stimulated by the parasympathetic nervous system, not in an arbitrary fashion, but in a way that optimizes gas exchange via the respiratory sinus arrhythmia, or synchronization of heart rate variability with respiration rate. This began to be measured in a number of care environments, and among newborns it was found to positively correlate with survival, particularly among premature newborns. This led to the conclusion at the time, in the early 90’s, that having a high vagal tone contributed to positive outcomes among newborns requiring intensive care. The trouble was that heart rate itself was still a relative marker of vagal tone or parasympathetic nervous system activity, and newborns, again especially the premature, had markedly worse outcomes and chances of survival if the exhibited a very low heart rate (also known and bradychardia). So on one hand you had respiratory sinus arrhythmia, indicating high vagal tone, found to be positively associated with survival in premature newborns; on the other hand you had premature infants with highly depressed heart rates, also an indicator of high vagal tone, to be associated with worse survival outcomes.
To resolve this apparent contradiction it was proposed that the parasympathetic nervous system innervated the heart through two dual pathways that function independently and antagonistically in the same way that the sympathetic and parasympathetic nervous system do.
In his book The Polyvagal Theory, published in 2011, Stephen Porges writes:
Premise 1: Neurogenic Bradycardia and RSA are mediated by different branches of the vagus and need not respond in concert….
Premise 2: Neurogenic bradycardia associated with orienting is a phylogenetic vestigial relic of the reptilian brain and is mediated by the [dorsomotor nucleus]….
Premise 3: Withdrawal of cardiac vagal tone through [nucleus ambiguus] mechanisms is a mammalian adaptation to select novelty in the environment while coping with the need to maintain metabolic output and continuous social communication.
What the above was mean to clarify was the reason the divergent functions of the VVC and the DVC appeared as they did in mammals, and consequently us.
A brief aside about reptiles and mammals.
Reptiles do not have any efferent neurons projecting from the nucleus ambiguus to the various targets in the head and thorax; they lack the VVC that mammals possess. Because reptiles are cold-blooded, they have much lower energy and oxygen requirements to stay alive than mammals do. Because of this the very low heart rate generated by the DVC is adaptive, and allows reptiles to conserve energy when needed at certain times.
Reptiles possess the same sympathetic nervous system structures that mammals do, including the sympatho-adrenal axis and hypothalimic-pituitary-adrenal axis, but it tends to see less use because reptiles, as a generalization, tend to use less active strategies for acquiring food.
Because of the lower activity of the sympathetic nervous system, the parasympathetic nervous system as the DVC also is used less.
Mammals do not have this luxury. Due to being warm-blooded and having much higher energy and oxygen requirements, their sympathetic nervous system is more active. To compensate for this the parasympathetic nervous system itself needs to be more active as well. The trouble with this is that the lowering of the heart rate using the slow, unmyelenated tracts of the DVC tends to depress the heart rate too low, resulting in insufficient oxygenation of the brain and resulting in death.
This is exactly what is seen in premature infants, whose VVC is insufficiently developed to provide a consistent vagal brake to the sympathetic nervous system and otherwise provide the necessary homeostatic regulation to compensate for fetal distress and sympathetic activation. At times when the regulation of the heart rate by the VVC is inconsistent, the body can compensate by using the DVC instead to lower the heart rate. Unfortunately this often lowers the heart rate too much and prevents the infant from receiving sufficient oxygen: an often life-threatening situation which requires intensive neonatal care. Because the VCC also innervates the mouth and lungs to coordinate swallowing with breathing, premature infants with a less developed VVC tend to have greater difficult with the sucking and swallowing actions needed to breastfeed properly also.
Concluding Thoughts
It is known from the Polyvagal Theory put forth by Dr Stephen Porges that the parasympathetic nervous system has two distinct branches, each with different functions and roles, even in cases where they innervate the same organs (e.g. heart and lungs).
If the distinction between the two systems was merely an academic one there would be no point in discussing it further. As it so happens, the separation of the parasympathetic response in the vagus nerve into two different subsystems has large implications in human behavior and in particular how our bodies deal with or more challenging forms of stress. Stay tuned for more.